Abbott Alinity c Cedia assay
Urine Clean plastic or glass container
2-8℃: 5 days
-20℃: longer
24 hours
ng/mL
Positivity Cut-Off: 10
6MAM heroin metabolite
Fluoroenzyme immunoassay (Phadia 250)
Tube Type:
Serum (Gold and red cap);
Heparin (Green cap) or EDTA (Lavender cap) Plasma
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT 7 days
7 days @ + 4ºC or longer @ -20 ºC
Phadia IFU & Eurofins Biomnis France
The ImmunoCAP Specific IgG is an immunoassay for the quantitative measurement of antigen specific IgG antibodies to A. fumigatus and A. flavus in serum. It is intended for in vitro diagnostic use to assess IgG associated immune response using Phadia 250 instrument.
Allergic bronchopulmonary aspergillosis (ABPA) and allergic bronchopulmonary mycosis (ABPM) involve the colonisation by Aspergillus fumigatus and other fungal species which elicit a characteristic humoral immune response to antigens or allergens of these fungi. A. fumigatus and A. flavus are opportunistic pathogens in humans. They can cause mild infections but also life-threatening diseases in those who are immunocompromised.
4 working days
mgA/L
<14 Negative
14-27 Equivocal
>27 Positive
All equivocal or positive screening result is to be confirmed by confirmatory technique.
According to a review of the literature, cut-offs in diseased population (ABPA or aspergillosis) vary between 27 and 50 mgA/L. A grey zone was defined for values between 14 and 27 mgA/L with 14 mgA/L representing the threshold
triggering confirmation of aspergillosis serology using the ASPERGILLOSIS IgG Western Blot (LDBIO).
ASPERGILLUS FUMIGATUS(M3) AND FLAVUS(M228) IGG
Stago Compact Max, Stago Satellite Max
Sodium Citrate Plasma 3.2%
Temperature: 4 hours Room temperature or 2 weeks -20ºC
Miscellaneous: N/A
Collection: Cf. Special requirement for Coagulation test
Whole blood: 4 hours, unless centrifuged at room temperature at 1500g for 15 min, separated and the plasma frozen. Can only be thawed once. If an expected delay from collection time to receipt in the laboratory, suggest send frozen plasma.
(BD Ref. VS5966 Evaluation of 0.109M BD Vacutainer® Plus Plastic and 0.105M BD Vacutainer® Glass Sodium Citrate Tubes for PT and APTT Using the Sysmex CA - 1500 Analyzer. BD, Franklin Lakes, NJ, USA June 2002; CSLI H21- A5)
Dacie and Lewis, Practical Haematology 12th edition, 2017
This test is also known as the Partial Thromboplastin Time with Kaolin (PTTK) and the Kaolin Cephalin Clotting Time (KCCT) reflecting the methods used to perform the test. The APTT is the main screening test for the Intrinsic clotting system and is the second most common coagulation test being exceeded in frequency only by the prothrombin time. The Partial Thromboplastin of the APTT is a phospholipid extract of animal tissue or from vegetable sources. The phospholipids act as a platelet substitute in the Intrinsic system. The test incorporates an activator, in the absence of added Thromboplastin, which shortens the test and increases the precision and reproducibility by eliminating the variable effects of contact from glass surfaces and by effecting maximum activation. The activator is used to stimulate the production of FXIIa by providing a surface for the function of high molecular weight Kininogen, Kallikrein and FXIIa. The contact activation occurs for a time at 37oC. Calcium is then added to trigger further reactions and the time required for clot formation measured. Standardised Phospholipids are required to form complexes, which activate FX and Prothrombin, which allows the test to be conducted in patient Platelet poor plasma (PPP). The test depends not only on the contact factors and factors VIII and IX, but also on the reactions with factors X, V, Prothrombin and Fibrinogen. It is also sensitive to the presence of circulating anticoagulants (inhibitors) and Heparin.
Preparation of patients: Patients should be relaxed pre-venepuncture. Excessive stress and exercise will increase Factor VIII, vWF antigen and fibrinolysis. Veno-occlusion should be avoided.
Precautions: APTT results may be affected by many commonly administered drugs and further studies should be made to determine the source of unexpected abnormal results. Oral contraceptive and Oestrogen therapy in males have been found to decrease APTT in vivo. Conversely, Heparin, Warfarin, Lupus anticoagulant and radio therapy have been found to increase APTT in vivo.
24 Hours
26.0 – 40 seconds
Activated partial thromboplastin time
Blood Sample
AffinityMap analyses maternal-fetal immunological compatibility by genotyping HLA-C and KIR genes. It assesses the risk of recurrent miscarriage, preeclampsia, and growth restriction due to immunological incompatibility, particularly when the embryo carries the paternal HLA-C2 allele and the maternal genotype is KIR AA.
Affinitymap is recommended for patients with recurrent miscarriage, implantation failure, or a history of or risk for preeclampsia, and can guide the selection of compatible sperm or egg donors.
18 days
Affinitymap
Abbott Alinity c Spectrophotometry NADH(without P-5'-P)
Serum: Serum Separator
Plasma: Di potassium EDTA Lithium heparin Lithium heparin separator Sodium heparin
Abbott:
20-25℃: 3 days
2-8℃: 7 days
-20℃: 60 days
Abbott IFU
24 hours
U/L
Abbott:
Adult Male < 45
Adult Female < 34
Alanine amino transferase alt
Abbott Alinity c Spectrophotometry (Bromocresol Green)
Serum : Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin
Potassium EDTA
Abbott:
20-25°C: 7 days
2-8°C: 7 days
-20°C: 3months
Abbott IFU
24 Hours
g/L
Abbott:
Adults: 35 - 50
60 – 90 years: 32 - 46
> 90 years: 29 - 45
Albumin
CALCULATION based on Abbott Alinity methodologies for Microalbumin and Urinary creatinine.
Urine spot/ timed/24hr: Clean, unused plastic or glass container with preservatives
20-25℃: 7 days
2-8℃: 7 days
-20℃: 1 year
NICE Guideline NG203, August 2021
24 Hours
ACR (Albumin/Creatinine Ratio): <3.0
Albumin/ creatinine ratio (ACR)
1mL : serum
Refridgerated
If you suspect allergy sensitization in a patient, a skin prick test or blood test will confirm the presence of allergen-specific IgE Antibodies.
The bottom-up approach to allergy diagnosis is where the patient is screened by using a very large panel to identify allergens that are not suspected from questioning the patient or from a skin prick test. Eurofins Biomnis offer this test to GPs.
IgE blood tests measure the presence of total and specific IgE allergens in the blood. Total IgE provides gross information. Specific IgE detects the presence of IgE antibodies that bind to the extract allergen or a molecular component. sIgE help to better define the IgE profile of a patient.
Advantages of a Blood test
- Results are not affected by histamine drugs
- It just requires a small blood draw and easier to work with children
- Dangerous allergens not administered to patients. No risk to patient.
- Automated work stations provide consistency in results
The top-down approach of allergy diagnosis is where the patient is seen by an allergist, skin prick tests are performed and then, if necessary, specific IgE tests for a selected panel of allergens are performed and then in some situations the study is deepened by using the likes of ALEX Allergy to have a very accurate picture of the IgE profile.
Advantages of Skin-Prick Test
- Faster results
- Skin-prick is more sensitive, IgE is more qualitative
2 Weeks
Alex Allergy
Abbott Alinity c Spectrophotometry Hydrolysis of Para- Nitrophenyl phosphate
Serum:
Serum separator
Plasma:
Lithium heparin
Lithium heparin separator
Sodium heparin
20-25℃: 7 days
2-8℃: 7 days
-20℃: 7 days
Abbott IFU
24 hours
U/L
16 to 21 years (Male): 56 - 167
22 to 79 years (Male): 50 - 116
16 to 29 years (Female):44 - 107
30 to 79 years (Female): 46 - 122
Alkaline phosphatase
Fluoroenzyme immunoassay on Phadia 250.
Serum (Red and gold cap); Heparin or EDTA Plasma (Green and Lavender cap)
Temperature: + 4ºC
Whole blood: RT unknown.
7 days @ + 4°C
Phadia Instructions for Use
Immunoglobulin E (IgE) specific to individual allergens is measured to determine which allergens are responsible for atopic symptoms and signs in an individual. The concentration of the specific IgE frequently correlates with the severity of symptoms. The following individual allergen specific IgEs are assayed at Eurofins Biomnis: E1, E3, E4, E5, D1, D2, F1, F2, F3, F4, F13, F14, F17, F18, F20, F25, F26, F27, F36, F44, F75, F81, F82, F83, F201, F245, F284, F343. The following panels are assayed: EX1, FX1, FX2, FX5, FX7, FX13, FX15, GX3, MX1, MX2, TX8, WX1, WX2. For details on these tests, see the Phadia Allergy website at http://www.phadia.com/Products/Allergy-testing-products/ImmunoCAPAllergen-Information/ (Accessed 22/05/20).
4 working days
Panels are reported as Positive or Negative only. Individual allergens are reported in kIU/L, ranging from less than 0.10 to greater than 100. A result of > 0.10 kIU/L is interpreted as positive.
Allergy testing: Phadia specific IGE
Abbott Alinity c Immunoturbidimetry
Serum :
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Sodium heparin
Potassium EDTA
Sodium citrate
2-8℃: 2 days
-20℃: not specified
24 hours
g/L
0.9 - 2.0
Alpha-1 antitrypsin A1AT
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
Serum, Serum separator.
Plasma:
Sodium heparin, Lithium heparin,
Dipotassium EDTA
Sodium EDTA
20-25℃: 3 days
2-8℃: 7 days
-20℃: longer
Abbott IFU
24 hours
IU/mL
Adult: 0.74 - 7.29
Alpha-fetoprotein AFP
Abbott Alinity c Homogeneous particle enhanced turbidimetric inhibition immunoassay (PETINIA).
Serum:
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin, Sodium heparin
K2-EDTA, K3-EDTA
2-8℃: 7 days
-20℃: 14 days
24 hours
mg/L
Trough: 4 - 8
Severe Infection (Peak): 25 - 35
Toxic Levels (Peak): >35
Amikacin
Abbott Alinity c Enzymatic Immunoassay
Urine Clean plastic or glass container
2-8℃: 5 days
-20℃: longer
Abbott IFU
24 hours
ng/mL
Positivity Cut-off: 1000
Amphetamine/meth amphetamine - urine
Abbott Alinity c Enzymatic + Colorimetric
Serum:
Serum tubes (with or without gel barrier)
Plasma:
Acceptable anticoagulants are: Lithium heparin Sodium heparin
20-25°C: 24 hr
2-8°C: 7 days
-20°C: 3 month
Abbott IFU
24 hours
U/L
Pediatric :
0-14 days: 3 - 10
15 day to < 13 week: 2 - 22
13 week to < 1 year: 3 - 50
1 year to < 18 year: 25 - 101
Adult:
28 - 100
Amylase
Abbott Alinity c Enzymatic/ Colorimetric Hydrolysis of Furylacryloylphenylalanylglyclglycine (FAPGG)
Serum is the preferred specimen.
Plasma:
Lithium heparin
Lithium heparin separator
Sodium heparin
20-25℃: 7 days
2-8℃: 7 days
-20℃: 1 year
Glenbio IFU
24 hours
U/L
>14 years: 8 - 65
Angiotensin converting enzyme (ace)
Fluoroenzyme immunoassay (Phadia 250)
Tube Type: Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT unknown;
14 days @ + 4ºC
Yes
The antiphospholipid syndrome (APS), also known as “Hughes syndrome”, is characterized by typical clinical features such as arterial/venous thromboses or recurrent miscarriages together with persistently positive tests for antiphospholipid antibodies. The criteria for classification of the APS have been revised in 2004 in Sydney. Besides the clinical criteria, three different laboratory tests are listed: lupus anticoagulant, anticardiolipin antibodies (IgG and IgM) and anti-β2-Glycoprotein I antibodies (IgG and IgM). The latter was not included in the former Sapporo criteria. However, by majority, the Sydney committee agreed that they are an independent risk factor for thrombosis and pregnancy complications. For APS diagnosis, β2-Glycoprotein I antibody tests show higher specificity than anticardiolipin assays. In 3-10% of APS patients, β2-Glycoprotein I antibodies may be the only positive test. The association of β2-Glycoprotein I antibodies with pre-eclampsia and/or eclampsia in unselected pregnant women who tested negative for anticardiolipin antibodies implies that the inclusion of β2-Glycoprotein I antibodies may also help clarify this type of pregnancy morbidity. Outside the context of clinical studies, testing for β2-Glycoprotein I antibodies can be helpful for APS diagnosis, particularly when anticardiolipin antibodies and lupus anticoagulant are negative and APS is strongly suspected.
4 working days
Negative: < 7.0 U/mL
Weak Positive: 7.0 U/mL to 10.0 U/mL
Positive: > 10.0 U/mL
Anti-B2-Glycoprotein 1 IGM Antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT unknown;
14 days @ + 4ºC
Source: Phadia IFU
The antiphospholipid syndrome (APS), also known as “Hughes syndrome”, is characterized by typical clinical features such as arterial/venous thromboses or recurrent miscarriages together with persistently positive tests for antiphospholipid antibodies. The criteria for classification of the APS have been revised in 2004 in Sydney. Besides the clinical criteria, three different laboratory tests are listed: lupus anticoagulant, anticardiolipin antibodies (IgG and IgM) and anti-β2-Glycoprotein I antibodies (IgG and IgM). The latter was not included in the former Sapporo criteria. However, by majority, the Sydney committee agreed that they are an independent risk factor for thrombosis and pregnancy complications. For APS diagnosis, β2-Glycoprotein I antibody tests show higher specificity than anticardiolipin assays. In 3-10% of APS patients, β2-Glycoprotein I antibodies may be the only positive test. The association of β2-Glycoprotein I antibodies with pre-eclampsia and/or eclampsia in unselected pregnant women who tested negative for anticardiolipin antibodies implies that the inclusion of β2-Glycoprotein I antibodies may also help clarify this type of pregnancy morbidity. Outside the context of clinical studies, testing for β2- Glycoprotein I antibodies can be helpful for APS diagnosis, particularly when anticardiolipin antibodies and lupus anticoagulant are negative and APS is strongly suspected.
4 working days
Negative: < 7.0 U/mL
Weak positive: 7.0 U/mL to 10.0 U/mL
Positive: > 10.0 U/mL
Anti-B2-glycoprotein 1 IGG antibodies
Chemiluminescent microparticle immunoassay (CMIA)
Chemiluminescent microparticle immunoassay (CMIA) technology
Serum (Gold and red cap); Plasma (lavender cap)
Temperature: + 4ºC
Miscellaneous: Non fasting
Serum (Gold and red cap);
Plasma (lavender cap)
Temperature: + 4ºC
Miscellaneous: Non fasting
≤3 days at 15-30 ºC
≤14 days at 2-8 ºC
>14 days at -20 ºC or colder.
≤3 days at 15-30 ºC
≤14 days at 2-8 ºC
>14 days at -20 ºC or colder.
Source: Abbott IFU
Source: Abbott IFU
Anti-HBc determinations can be used to monitor the progress of hepatitis B viral infection. Anti-HBc is found in serum shortly after the appearance of Hepatitis B Surface Antigen (HBsAg) in acute hepatitis B infections. It will persist after the disappearance of HBsAg and before the appearance of detectable antibody to HBsAg (anti-HBs).
In the absence of information about any other hepatitis B virus (HBV) markers, it must be considered that an individual with detectable levels of anti-HBc may be actively infected with HBV or that the infection may have resolved, leaving the person immune. Anti-HBc may be the only serological marker of hepatitis B viral infection and potentially infectious blood. The presence of anti-HBc does not differentiate between acute or chronic hepatitis B infections.
Preparation of Patient: There is no special physical preparation for the test.
1 working day
1 working day
Specimens with S/CO values < 1.00 are considered Non-reactive (NR).
Specimens with S/CO values >= 1.00 are considered reactive (R).
This is a screening test and reactive samples will be referred to NVRL for confirmatory testing.
Anti-Hepatitis B core antibody
Chemiluminescent microparticle immunoassay (CMIA)
Chemiluminescent microparticle immunoassay (CMIA)
Serum (Gold and red cap);
Plasma (lavender cap)
Temperature: + 4ºC
Miscellaneous: Non-fasting
Serum (Gold and red cap);
Plasma (lavender cap)
Temperature: + 4ºC
Miscellaneous: Non fasting
Whole blood ≤ 14 days at 2-8°C.
Separated: >14 days frozen (-20°C or colder)
Whole blood ≤ 14 days at 2-8°C.
Separated: >14 days frozen (-20°C or colder)
Source: Abbott IFU
For further guidance re. immunisation protocols and testing see https://www.hse.ie/eng/health/immunisation/hcpinfo/guidelines/chapter9.pdf
Source: Abbott IFU
For further guidance re. immunisation protocols and testing see https://www.hse.ie/eng/health/immunisation/hcpinfo/guidelines/chapter9.pdf
Anti-HBs is a specific antibody directed against the hepatitis B surface antigen. Anti-HBs can be formed following a Hepatitis B infection or after a Hepatitis B vaccination. This test is used within the scope of hepatitis B vaccination to check the necessity and success of vaccination. Moreover, anti-HBs tests are used to monitor the course of disease following acute hepatitis B infection.
Preparation of Patient: There is no special physical preparation for the test.
1 working day
1 working day
mIU/ml <10 : Non reactive /Non-Immune
If post-vaccination, patient is a nonresponder. Test for Anti-HBc. If anti-HBc negative, give booster dose of the same hepatitis B vaccine. Recheck anti-HBs 2 months later and if anti-HBs remains <10
mIU/ml, give two further doses of the same hepatitis B vaccine (i.e. complete a second course of the same hepatitis B vaccine).
Recheck anti-HBs 2 months later and if anti-HBs remains <10 mIU/ml, person is susceptible to HBV.
≥ 10: Reactive/Immune
Based on the World Health Organisation and NIAC recommendations, an Anti-HBs concentration ≥ 10 mIU/mL is regarded as being protective against Hepatitis B viral infection.
Anti-Hepatitis B surface antibody
Roche Cobas e602 Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
1mL Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin
20-25°C: 3 days
2-8°C: 5 days
-20°C: 6 months
Roche IFU
AMH provides information about a woman’s ovarian reserve providing insight into the quantity not the quality of the eggs. Antral follicle count (AFC), via a transvaginal ultrasound, is the gold standard for determining a women’s egg count, AMH concentrations correlate with AFC. AMH is also beneficial in gynaecology in granulosa tumour diagnosis.
Currently, age is the strongest predictor in estimating egg quality. Beyond age, genetics, exposure to chemotherapy and radiation, and certain medical conditions can also influence ovarian reserve. Fewer eggs mean fewer chances for conceiving a baby.
Beneficial in paediatric endocrinology particularly in the case of müllerian duct persistence syndrome, a rare form of sexual ambiguity.
4 Days
pmol/L
Female 20-24 years: 8.71 - 83.6
Female 25-29 years: 6.35 - 70.3
Female 30-34 years: 4.11 - 58.0
Female 35-39 years: 1.05 - 53.5
Female 40-44 years: 0.193 - 39.1
Female 45-50 years: 0.071 - 19.3
PCOS Women: 13.3 - 135
Healthy Men: 5.5 - 103
Anti-Mullerian Hormone AMH
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator
Plasma: Lithium heparin
Potassium EDTA
20-25℃: 8hours
2-8℃: 72 hours
-20℃: 30 days
Abbott IFU
24 hours
IU/mL
Adults: < 4.11
Anti-TG
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator
Plasma: Lithium heparin
Potassium EDTA
20-25℃: 8 hours
2-8℃: 72 hours
-20℃: 30 days
Abbott IFU
24 hours
IU/mL
Adults: < 5.61
Anti-TPO
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (EDTA, Citrate).
Heparin plasma is NOT suitable.
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT unknown.
14 days @ + 4ºC
Phadia IFU
Celiac disease is a life-long condition in which ingestion of gluten, the water insoluble wheat gliadin and the prolamins in rye and barley, leads to chronic inflammation and damage of the small intestinal mucosa. Tissue transglutaminase has been identified as the major autoantigen in celiac disease. IgA antibodies against tTG are highly disease specific serological markers for celiac disease and dermatitis herpetiformis. tTG IgG antibodies are less specific for these diseases but are helpful markers in patients with IgA deficiency.
Preparation of Patient: No special preparation.
4 working days
Negative: less than 7 U/mL
Weak Positive: 7 - 10 U/mL
Positive: greater than 10 U/mL
Anti-Transglutaminase IGA antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT 1 day.
14 days @ + 4ºC
Source: Phadia IFU
Anti-cardiolipin antibodies (ACA) belong to the group of anti-phospholipid antibodies (aPL). Their occurrence was first demonstrated in sera of syphilis patients, but later they have also been described frequently in SLE (systemic lupus erythematosus) patients (prevalence 30-40%) and in patients with other rheumatic diseases. The antiphospholipid syndrome (APS), also known as “Hughes syndrome”, is characterized by typical clinical features such as arterial/venous thrombosis or recurrent miscarriages together with persistently positive tests for aPL. In contrast to “secondary APS” which occurs in association with SLE or other rheumatic disorders, there is no evidence for another relevant underlying disease in primary APS. New criteria for classification of the antiphospholipid syndrome have been defined recently.
Anti-cardiolipin antibodies in infectious diseases and in APS can be distinguished with respect to their dependence on cofactors: whereas ACA from patients with infectious diseases recognize the pure phospholipid as antigen, binding of ACA from patients with APS requires β2-glycoprotein I as a cofactor. For this reason, ACA ELISAs need β2- glycoprotein I to be incorporated into the assay.
The so-called ‘lupus anticoagulant' (LA) describes a phenomenon that is related to the presence of antiphospholipid antibodies. It is defined by the measurement of antibody dependent coagulation inhibition in vitro. ACA/LA are considered to be of significant diagnostic relevance, as a correlation has been found between these antibodies and a tendency towards thromboses. This results in an increased incidence of venous/arterial thromboses, thrombocytopenia, livido reticularis, habitual abortion and neurological manifestations in ACA/LA-positive patients. Elevated levels of ACA/LA may also be found in patients with cerebrovascular insufficiency or myocardial infarction. aPL are thought to play a direct role in the pathogenesis of APS.
Preparation of Patient: No special preparation.
4 working days
Negative: < 10.0 GPL-U/mL
Weak positive: 10.0 - 40.0 GPL-U/mL
Positive: > 40.0 GPL-U/mL
Anti-cardiolipin IGG antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap)
Whole blood: unknown.
Separated: RT 1 day.
14 days @ + 4ºC
Phadia IFU
Anti-cardiolipin antibodies (ACA) belong to the group of anti-phospholipid antibodies (aPL). Their occurrence was first demonstrated in sera of syphilis patients, but later they have also been described frequently in SLE (systemic lupus erythematosus) patients (prevalence 30-40%) and in patients with other rheumatic diseases. The antiphospholipid syndrome (APS), also known as “Hughes syndrome”, is characterized by typical clinical features such as arterial/venous thrombosis or recurrent miscarriages together with persistently positive tests for aPL. In contrast to “secondary APS” which occurs in association with SLE or other rheumatic disorders, there is no evidence for another relevant underlying disease in primary APS. New criteria for classification of the antiphospholipid syndrome have been defined recently.
Anti-cardiolipin antibodies in infectious diseases and in APS can be distinguished with respect to their dependence on cofactors: whereas ACA from patients with infectious diseases recognize the pure phospholipid as antigen, binding of ACA from patients with APS requires β2-glycoprotein I as a cofactor. For this reason, ACA ELISAs need β2- glycoprotein I to be incorporated into the assay.
The so-called ‘lupus anticoagulant' (LA) describes a phenomenon that is related to the presence of antiphospholipid antibodies. It is defined by the measurement of antibody dependent coagulation inhibition in vitro. ACA/LA are considered to be of significant diagnostic relevance, as a correlation has been found between these antibodies and a tendency towards thromboses. This results in an increased incidence of venous/arterial thromboses, thrombocytopenia, livido reticularis, habitual abortion and neurological manifestations in ACA/LA-positive patients. Elevated levels of ACA/LA may also be found in patients with cerebrovascular insufficiency or myocardial infarction. aPL are thought to play a direct role in the pathogenesis of APS.
Preparation of Patient: No special preparation.
4 working days
Negative: < 10.0 MPL-U/mL
Weak positive: 10.0 - 40.0 MPL-U/mL
Positive: > 40.0 MPL-U/mL
Anti-cardiolipin IGM antibodies
Abbott Alinity. CMIA.
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Serum/Plasma: RT 22 hours,
2-8ºC 7 days.
>7 days @ -20ºC
Abbott IFU
Rheumatoid Arthritis (RA) is a common, systemic autoimmune disease affecting 0.5-1% of the population. It is characterized by chronic inflammation of the synovium, which commonly leads to progressive joint destruction and in most cases, to disability and reduction of quality of life. Evidence gained over the last few years suggests that aggressive therapy given early in the disease has the greatest therapeutic potential.
The serum of RA patients contains a variety of antibodies directed against self-antigens. The most widely known of these autoantibodies is the rheumatoid factor (RF) antibody directed against the constant domain of IgG molecules. The presence of RF is one of the American College of Rheumatology’s criteria for the classification of RA. Although the RF test has good sensitivity for RA, it is not very specific for the disease as it can also be detected in the serum of patients with other rheumatic or inflammatory diseases and even in a substantial percentage of the healthy (elderly) population. For several years it has been recognized that antibodies to anti-perinuclear factor and anti-keratin are highly specific for RA. It was subsequently reported that both of these antibodies reacted with native filaggrin and are now referred to as anti-filaggrin antibodies. More recently it has been shown that all of these antibodies are directed to citrulline-containing epitopes. Citrulline is a nonstandard amino acid, as it is not incorporated into proteins during protein synthesis. It can, however, be generated via post-translational modification of arginine residues by the enzyme peptidyl arginine deiminase. In 1998, Schellekens and colleagues reported that linear peptides containing citrulline (CP) were very specific for RA antibodies (96%) in an ELISA based assay. Subsequent work demonstrated that cyclic variants of these peptides, termed cyclic citrullinated peptides (CCP), were equally specific for RA, but with a higher sensitivity than linear peptides. To improve the sensitivity of the CCP test further, several dedicated libraries of citrulline-containing peptides were screened with RA sera and a new set of peptides (CCP2) were discovered which gave superior performance compared to the CCP1 test. Over the last few years, many independent studies have confirmed the diagnostic performance of the CCP2 test. In 2007, the European League against Rheumatism (EULAR) published guidelines for the diagnosis of early RA, and the measurement of antibodies to anti-CCP was included as a serology marker.
Preparation of Patient: No special preparation.
4 working days
Negative: < 5.0 U/mL
Positive: ≥ 5.0 U/mL
Anti-cyclic citrullinated peptide antibodies
Fluoroenzyme immunoassay (Phadia 250) EliA GliadinDP IgA
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown
Separated: RT unknown,
14 days @ + 4ºC
Phadia IFU
Coeliac disease is a life-long condition in which ingestion of gluten, the water insoluble wheat gliadin and the prolamins in rye and barley, leads to chronic inflammation and damage of the small intestinal mucosa. The disease is multifaceted in nature with clinical presentation ranging from gastrointestinal manifestations to asymptomatic, silent and extraintestinal forms. It is widely accepted that dermatitis herpetiformis, a bullous skin disease, is induced by gluten. The term gluten refers to a whole set of proteins in the socalled endosperm, the nutritive tissue of the grain seed of wheat, rye, oats and barley. The alcohol-soluble polypeptides of gluten, the gliadins, are solely responsible for the toxic effects to the intestinal mucosa. More recent research revealed that gliadin peptides deamidated by tissue transglutaminase represent more specific B-cell epitopes than native peptides.
4 working days
Negative: < 7.0 U/mL
Borderline: 7.0 - 10.0 U/mL
Positive: > 10.0 U/mL
Anti-gliadin IGA antibodies
Fluoroenzyme immunoassay (Phadia 250) EliA GliadinDP IgG
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown
Separated: RT unknown,
14 days @ + 4ºC
Phadia IFU
Coeliac disease is a life-long condition in which ingestion of gluten, the water insoluble wheat gliadin and the prolamins in rye and barley, leads to chronic inflammation and damage of the small intestinal mucosa. The disease is multifaceted in nature with clinical presentation ranging from gastrointestinal manifestations to asymptomatic, silent and extraintestinal forms. It is widely accepted that dermatitis herpetiformis, a bullous skin disease, is induced by gluten. The term gluten refers to a whole set of proteins in the socalled endosperm, the nutritive tissue of the grain seed of wheat, rye, oats and barley. The alcohol-soluble polypeptides of gluten, the gliadins, are solely responsible for the toxic effects to the intestinal mucosa. More recent research revealed that gliadin peptides deamidated by tissue transglutaminase represent more specific B-cell epitopes than native peptides.
4 working days
Negative: < 7.0 U/mL
Weak positive: 7.0 - 10.0 U/mL
Positive: > 10.0 U/mL
Anti-gliadin IGG antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT unknown
14 days @ + 4ºC
Phadia IFU
GBM antibodies occur in patients suffering from Goodpasture syndrome, anti-GBMdisease and ANCA associated vasculitis. Goodpasture syndrome is defined by the combined occurrence of progressive glomerulonephritis, lung haemorrhage and antibodies to the glomerular basement membrane (GBM). A more limited form only involving the kidney or the lung is referred to as anti-GBM disease. For the diagnosis of both, Goodpasture syndrome and anti-GBM-disease, the presence of GBM antibodies is required. Furthermore up to 10 % of ANCA positive patients show GBM antibodies, which indicate a more severe course of renal damage.
4 working days
Negative: < 7.0 U/mL
Weak positive: 7.0 - 10.0 U/mL
Positive: > 10.0 U/mL
Anti-glomerular basement membrane antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT 8 hours;
14 Days @ + 4ºC
Phadia IFU
Pernicious anaemia (also known as Biermer’s disease) is an autoimmune atrophic gastritis, predominantly of the fundus, and is responsible for a deficiency in vitamin B12 (cobalamin) due to its malabsorption. Its prevalence is 0.1% in the general population and 1.9% in subjects over the age of 60 years. Pernicious anaemia represents 20%–50% of the causes of vitamin B12 deficiency in adults. Anti intrinsic factor antibodies do not appear to have a clearly defi ned pathogenic role in the development of gastritis. By contrast, they have a well-documented role in the onset of pernicious anaemia, via the vitamin B12 deficiency they induce. The finding of a low total serum cobalamin level may be further evaluated by testing for anti-intrinsic factor antibodies. If positive, the antibodies have a high positive predictive value (95%) for the presence of pernicious anaemia with a concurrent low false positive rate (1–2%) i.e. a high specificity. It identifies those patients with a need for lifelong cobalamin replacement therapy.2 With regard to diagnostic performance sensitivity is low for anti-intrinsic factor antibodies, in the most recent studies while specificity is 100%. In combination with anti-parietal cell antibodies they yield 73% sensitivity and 100% specificity.
Preparation of Patient: No special preparation.
4 working days
Negative: less than 7 U/mL
Equivocal: 7 - 10 U/mL
Positive: greater than 10 U/mL
Anti-intrinsic factor antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT 8 hours;
14 Days @ + 4ºC; months at - 20 ºC
Phadia IFU
Primary biliary cirrhosis (PBC) is a chronic, cholestatic liver disease which affects mainly middle-aged women. It starts with an inflammatory process of the small and middle-sized interlobular bile ducts leading first to a proliferation and then to a loss of bile ducts, to portal inflammation and in late stages to liver cirrhosis.
PBC occurs all over the world but with varying incidence, ranging from 0.7-49 per million per year. In most recent studies the point prevalence was estimated to range from 6.7 to 402 per million.
Typical clinical features of PBC are fatigue, pruritus and Sicca-syndrome. However, nowadays at diagnosis, the majority of patients are asymptomatic and present for other reasons, e.g. for workup of elevated serum levels of AP or cholesterol. A diagnosis of PBC is made “with confidence” when biochemical markers of cholestasis, particularly alkaline phosphatase, are elevated persistently for more than 6 months in the presence of antibodies against mitochondria and in the absence of an alternative explanation.
PBC-related antibodies against mitochondria react with subunits of the 2-oxoaciddehydrogenase complex (2-OADC) and, in most cases, recognize the E2-subunit of pyruvate dehydrogenase (PDH-E2). Individuals, who are positive for these so-called antiM2 antibodies, even if they have no signs of cholestasis and/or liver inflammation, are very likely to develop PBC.
Anti-M2 antibodies are present in about 95% of PBC-patients.
Preparation of Patient: No special preparation.
4 working days
Negative: < 4.0 IU/mL
Equivocal: 4.0 IU/mL to 6.0 IU/mL
Positive: > 6.0 IU/mL
Anti-m2 anti-mitochondrial antibodies
Chemistry – Fluoroenzyme immunoassay.
Serum (Red and gold cap); Plasma (Green and lavender cap). Lipaemic and haemolysed samples are unsuitable.
Temperature: + 4ºC
Whole blood: unknown
Separated: RT unknown;
14 days @ + 4ºC
Phadia IFU
First described in patients with necrotizing crescentic glomerulonephritis (NCGN) without immune deposits (pauci-immune), the clinical spectrum associated with anti-MPO includes also NCGN associated with systemic vasculitis, either Granulomatosis with polyangiitis (GPA) or a microscopic polyangiitis (MPA). Indeed, anti-MPO are detectable in 65% of patients with idiopathic NCGN, 45% of patients with MPA and 20% to 30% of patients with GPA. Additionally, anti-MPO are present in some 60% of patients with the eosinophilic granulomatosis with polyangiitis (EGPA). Antibodies to PR3 are highly sensitive (81%) and specific (97%) for GPA. The sensitivity is dependent on the phase and on the activity of the disease. Despite the strong association between PR3 antibodies and GPA, there is a small percentage of patients with microscopic polyangiitis and about 30% of EGPA patients who are PR3 antibodies positive. PR3 antibodies may also occur in 20% to 30% of patients with necrotizing glomerulonephritis with no obvious extrarenal manifestations of small vessel vasculitis.
Preparation of Patient: There is no special physical preparation required.
4 working days
Anti-MPO: less than 3.5 IU/mL (<3.5 = negative; 3.5-5.0 = equivocal; >5.0 = positive)
Anti-PR3: less than 2.0 IU/mL (<2.0 = negative; 2.0-3.0 = equivocal; >3.0 = positive)
Anti-mpo and Anti-pr3 antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap).
Temperature: + 4ºC
Whole blood: unknown
Separated: RT unknown;
14 days @ + 4ºC
Phadia IFU
The determination of antinuclear antibodies (ANA) is of central importance for the clinical diagnosis of connective tissue diseases, which are systemic inflammatory diseases with a chronic course of disease. Connective tissue diseases exhibit overlapping symptomatic features that render an accurate diagnosis difficult.
The Phadia EliA ANA CTD screen wells are coated with human recombinant U1RNP (RNP70, A, C),SS-A/Ro (60 kDa, 52 kDa), SS-B/La, Centromere B, Scl-70, Jo-1, Fibrillarin, RNA Pol III, Rib-P, PM-Scl, PCNA, Mi-2 proteins, Sm proteins and native purified DNA. This ANA screen is more specific than traditional IF ANA methods, which show a high false positive rate.
A positive ANA CTD screen requires the specific quantification of the antibodies listed above: ds-DNA and the individual anti-extractable nuclear antigen (ENA) antibodies.
For the diagnosis of systemic lupus erythematosus (SLE), dsDNA antibodies are considered to be a highly specific marker representing one of the diagnostic criteria for SLE (ACR criteria). More than 90 % of sera from patients with active SLE contain dsDNA antibodies. Additionally, the determination of dsDNA antibodies is a tool to monitor the clinical course of a defined SLE patient, because a clear-cut relationship exists between anti-dsDNA titre and disease activity, in particular renal involvement. Sm antibodies offer a highly specific, but comparatively insensitive, clinical marker for SLE. Indeed, their presence constitutes one of the revised ACR criteria for diagnosis, even though their overall prevalence ranges from 20 % to 30 % in SLE. U1-snRNP antibodies typically appear in both SLE and mixed connective tissue disease (MCTD, Sharp Syndrome).
In MCTD, the presence of U1-snRNP antibodies is required for diagnosis, whereas they occur in only 30 to 40 % of SLE patients. Detection of SS-A/Ro antibodies is of interest and significance for the clinical diagnosis of SLE (prevalence 40-50%) and Sjögren's syndrome (prevalence 60-75% for primary Sjögren's syndrome). They have been reported to occur in tight association with certain disease subsets, such as subacute cutaneous LE, neonatal lupus erythematosus or vasculitis in Sjögren's syndrome. As anti-SS-A/Ro may be the only antibody present in many patients with SLE or Sjögren's syndrome, failure to measure antiSS-A/Ro leaves a diagnostic void which cannot be filled by other tests. SS-B/La antibodies are the serological hallmark of Sjögren's syndrome but a small proportion of patients remains anti-SS-B/La negative. La antibodies are found in 6-15 % of sera from SLE patients. Here, they are associated with a lower prevalence of dsDNA antibodies and renal disease.
Although a strong association of neonatal lupus erythematosus (NLE) with Ro antibodies was recognized first, the majority of mothers with babies with NLE are now known to have La antibodies as well.
CENP antibodies are found in 70-90 % of patients with CREST Syndrome, a limited form of scleroderma with a comparatively favourable prognosis. However, they may also occur in Raynaud's phenomenon and primary biliary cirrhosis (about 10-20 %).
Antibodies against Scl-70 are characteristic and specific for scleroderma (particularly the diffuse form; frequency up to 70%). Jo-1 antibodies can be found as markers in dermatomyositis/polymyositis (prevalence of about 25%), but also in patients with polymyositis overlap syndrome. They are associated with interstitial pneumonitis (in the context of myositis) and occur in a far smaller proportion of children with myositis than of adults. Patients with Jo-1 antibodies tend to have a severe form of the disease with a tendency to relapse and a poorer prognosis. Fibrillarin antibodies produce a nucleolar pattern in immunofluorescence. They occur in less than 15% of patients with scleroderma and seem to be associated with internal organ involvement including pulmonary hypertension, myositis, and renal disease. The presence of fibrillarin antibodies in diseases other than scleroderma and their clinical relevance requires further investigation. RNA polymerase III antibodies are highly specific for scleroderma and are here more frequent in patients with diffuse cutaneous scleroderma than in those with limited cutaneous scleroderma. Among patients with diffuse cutaneous involvement, RNA polymerase III antibody was the most common antibody detected (35-45%).
Antibodies against Ribosomal P proteins react with the specific ribosomal proteins (P0, P1 and P2). These autoantibodies occur in SLE during active disease and are associated with neuropsychiatric, renal and hepatic involvement. They are found in 23% of SLE patients.
Autoantibodies to the polymyositis/scleroderma (PM-Scl) complex were the first antinucleolar antibodies identified in systemic sclerosis. Anti-PM-Scl are associated with a specific form of scleroderma; indeed, only 2% of the patient population with scleroderma, but 24% of the patients with myositis-scleroderma overlap syndrome produce these antibodies. They correlate with a benign course of disease and a positive response to steroid therapy. Antibodies against PCNA (proliferating cell nuclear antigen) occur in 2 to 10% of SLE patients but seem to be not very specific for SLE as it was found in 12.3% of hepatitis B and 18.7% of hepatitis C patients, respectively.
Autoantibodies targeting the Mi-2 nuclear antigen represent one of the serologic hallmarks of polymyositis/dermatomyositis, with a diagnostic sensitivity and specificity of approximately 4-18% and 98-100%, respectively. They are strongly associated with dermatomyositis with a frequency of up to 31%.
Preparation of Patient: No special preparation.
Reflex testing: The Phadia EliA ANA CTD wells are coated with human recombinant U1RNP (RNP70, A, C),SS-A/Ro (60 kDa, 52 kDa), SS-B/La, Centromere B, Scl-70, Jo-1, Fibrillarin, RNA Pol III, Rib-P, PM-Scl, PCNA, Mi-2 proteins, Sm proteins and native purified DNA. A positive ANA CTD screen will lead to analysis of specific ds-DNA antibodies and ENA antibody typing.
4 working days
ANA: ratio less than 0.7
ds-DNA: less than 10 IU/mL
Anti-Sm, anti-SSA/RO, anti-SSB/La, anti-Scl-70, anti-Jo-1 and anti-centromere Antibodies: each less than 7 EliA U/mL.
Anti-U1 RNP: less than 5 EliA U/mL.
Anti-nuclear antibodies, DS-DNA and ENA antibodies
Fluoroenzyme immunoassay (Phadia 250)
Serum (Gold and red cap); Plasma (green and lavender cap)
Temperature: + 4ºC
Whole blood: unknown.
Separated: RT 8 hours;
14 Days @ + 4ºC
Phadia IFU
Pernicious anaemia (also known as Biermer’s disease) is an autoimmune atrophic gastritis, predominantly of the fundus, and is responsible for a deficiency in vitamin B12 (cobalamin) due to its malabsorption. Its prevalence is 0.1% in the general population and 1.9% in subjects over the age of 60 years. Pernicious anaemia represents 20%–50% of the causes of vitamin B12 deficiency in adults. Parietal cell antibodies are found in about 90% of Caucasian patients with pernicious anaemia. In the later stages of the disease, the incidence of these antibodies decreases due to the progression of autoimmune gastritis and a loss of parietal cell mass, as a result of the decrease in antigenic rate. In recent studies, an average incidence of 55% of anti-parietal cell antibodies was documented in patients with advanced pernicious anaemia. Parietal cell antibodies are present in 7.8–19.5% of the general healthy adult population. A not fully explained question is whether parietal cell antibodies presence is related to Helicobacter pylori infection. Anti-parietal cell antibodies are found in up to 20.7% of these patients.
Preparation of Patient: No special preparation.
4 working days
Negative: less than 7 U/mL
Equivocal: 7 - 10 U/mL
Positive: greater than 10 U/mL
Anti-parietal cell antibodies
Turbidimetric/Immunoturbidimetric
Serum (Gold and red cap).
Temperature: + 4ºC
Miscellaneous: Non fasting
Serum
≤2 days at 2-8 ºC
> 2 days -20 ºC
Source: Abbott IFU
The group A β-haemolytic streptococci produce various toxins that can act as antigens. One of these exotoxins is streptolysin-O. The affected organism produces specific antibodies against these exotoxins, among which concentration of Anti-Streptolysin-O in the patient’s serum will enable to establish the degree of infection due to the β-haemolytic streptococcus.
A positive test can indicate recent or current group A, C, and G streptococcal infection (e.g., upper airway infections, scarlet fever, toxic shock syndrome) and may support the diagnosis of post-streptococcal infection complication (e.g., glomerulonephritis and rheumatic fever).
The test is positive in only 80-85% of group A streptococcal infections, so a negative test does not necessarily exclude the diagnosis.
Preparation of Patient: There is no special physical preparation for this test.
1 working day
Up to 7 years: less than 100 IU/mL
Greater than 7 years: less than 200 IU/mL
Anti-streptolysin o titre (ASOT)
Abbott Alinity c Spectrophotometry
Serum:
Serum Separator
Plasma:
Lithium heparin
Lithium heparin separator
Sodium heparin
20-25℃: 4 days
2-8℃: 7 days
-20℃: 3 months
Abbott IFU
24 hours
U/L
Adults: 11- 34
Aspartate amino transferase AST
Abbott Alinity c Enzymatic Immunoassay
Urine Clean plastic or glass container
2-8℃: 5 days
-20℃: longer
Abbott IFU
24 hours
ng/mL
Positivity Cut-off: 200
Barbiturates, semiquantitative
Abbott Alinity c Enzymatic Immunoassay
Urine Clean plastic or glass container
2-8℃: 5 days
-20℃: longer
Abbott IFU
24 hours
ng/mL
Positivity Cut-off: 200
Benzodiazepines semiquantitative
Abbott Alinity c Turbidimetric/ Immunoturbidimetry
Plasma Collection tubes Acceptable anticoagulants are: EDTA Sodium heparin
20-25℃: 7 days
2-8℃: 7 days
-20℃: 1 year
Abbott IFU
24 hours
mg/L
Adults: 0.97 - 2.64
Beta-2-microglobulin
Abbott Alinity c Cyclic-enzymatic/ colorimetric
Serum Plastic tubes (with or without gel barrier)
20-25°C: 1 day
2-8°C: 7 days
Abbott IFU
24 hours
µmol/L
Adult: 1.0 - 6.0
Pregnancy: 1.3 - 9.0
Bile acid
Abbott Alinity c Spectrophotometry, Diazo-Reaction
Serum:
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin (with or without gel barrier)
Sodium heparin
EDTA
20-25℃: 2 days
2-8℃: 7 days
-20℃: 3 months
Abbott IFU
24 hours
µmol/L
Adult: 0.0 - 8.6
Bilirubin direct
Abbott Alinity c Spectrophotometry, Diazonium salt
Serum: Serum separator
Plasma: Lithium heparin and Lithium heparin separator
Sodium heparin
Dipotassium EDTA
20-25°C: 8 hr
20-25°C: 24 hr (serum separator and Lithium heparin separator)
2-8°C: 7 days -20°C: 3 mth
Abbott IFU
24 Hours
µmol/L
Premature:
0 - 1day <136.8 1-2 day <205.2 3-5 day <273.6
Full-term
0 - 1day 34.2 - 102.6 1-2 day 102.6 - 171 3-5 day 25.7 - 205.2
Premature: Full-term Adult
5.1 - 20.5
Bilirubin total
CALCULATION based on Abbott Alinity methodologies for Total Bilirubin and Direct Bilirubin
Serum:
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin, Sodium heparin, EDTA
20-25℃: 8 hours
2-8℃: 7 days
-20℃: 3 months
Abbott IFU
24 hours
Adult: 3.0 - 12.0
Bilirubin, indirect
Manual microscopy
Whole Blood K2/K3 EDTA anticoagulated or unstained blood smears prepared from such specimens.
Temperature: + 2-8ºC for whole blood. Unstained slides can also be stored at room temperature.
Miscellanous: N/A
48 hours @ + 2-8ºC for whole blood.
8 weeks for blood smear slides prepared from whole blood EDTA anticoagulated specimens meeting the above stability criteria.
Blood film review remains an indispensable diagnostic tool, despite advances in automated technologies. The blood film, or peripheral blood smear, allows for the direct visualisation of blood cells, providing insights that are often beyond the reach of automated analysers. Automated analysers, while efficient, can miss subtle morphological abnormalities such as dysplastic changes, reactive features, atypical cells, or early signs of malignancies. In some cases, the blood film review is the only reliable methodology to identify key disease associated markers. For instance, the presence of schistocytes in microangiopathic haemolytic anaemia can only be reliably identified through a manual smear review. Blood film review thus aids in the differential diagnosis of patients presenting with haematological abnormalities which cannot be detected through routine automated methods.
In addition to its role in patient diagnosis, blood film review plays an essential role in the detection of spurious FBC results caused by pre-analytical artefacts or sample handling. For example, the clumping of platelets in EDTA anticoagulated samples may lead to spurious reporting of thrombocytopaenia.
At Eurofins-Biomnis Ireland, blood film review is provided as part of the FBC package and is automatically requested based on FBC result criteria.
Preparation of patients: There is no physical preparation for the blood film review.
Precautions: Frozen, clotted, or grossly haemolysed samples cannot be analysed.
24 hrs
Blood Film Review
Haematology – Thick & Thin Blood film & CareStart Malaria Rapydtest antigen kit (Kit Insert:
APACOR CareStart RAPYDTEST- APA059 V7 04/2017)
Whole Blood K2/K3 EDTA (Lavender cap)
Temperature: + 2-8ºC
Miscellaneous: Observe periodicity where applicable.
Blood films Thick & thin need to be made less than 2 hours after the blood EDTA was drawn.
WHO Guideline: ‘The Laboratory Diagnosis of Malaria’. J.W Bailey, B.J Bain, J Parker-Williams and P.Chiodini for the General Haematology Task Force of the British Committee for Standards in Haematology. http://www.bcshguides.com/documents/malaria-bcsh.2005.pdf
Malaria Reference Laboratory. www.malaria-reference.co.uk
Malaria is caused by a group of related intracellular protozoan pathogens of the genus Plasmodium. These species exhibit a complex life cycle reliant on a mammalian host and anopheles mosquito vector. In the human host they are obligate intracellular pathogens infecting initially the liver in the sporozoite form. In the liver the parasites replicate and develop into merozoites which are then released into the blood stream. These infect the erythrocyte and begin a restricted life cycle. Each parasite may develop into a schizont (a cluster of infectious units which may invade further erythrocytes) or a gametocyte (the sexual form which may be transferred to the anopheles mosquito upon taking a blood meal). Re-infection of the liver does not occur.
Suspected malaria is a medical emergency. Sampling and processing of the blood sample must not be delayed if malaria is suspected. Five primary species of malaria have been identified in humans: P.falciparum, P.vivax, P.ovale P.malariae and P.knowlesi. Their geographic distribution is unique for each species.
Blood should ideally be taken direct from the patient’s finger or ear & the films prepared at the bedside or in the clinic. When this is not possible blood taken into anticoagulant (EDTA) can be used. Thick & thin blood films should be made as soon as possible, certainly less than 2 hours after the EDTA blood was drawn, to minimise morphological changes in the parasites. Parasite and red cell morphology can be seriously affected if the blood has been in anticoagulation for too long.
Where there is a strong clinical suspicion if the first films are negative, blood should be taken and films made and checked at least two times over the first 24 hours and further films examined every 12 hours after that if strongly clinically indicated.
Preparation of patients:
Travel history should be recorded, and any clinical details recorded on the request form.
In symptomatic patients please phone the laboratory prior to sending the sample.
Precautions: Global distribution of malaria is restricted to areas endemic to the anopheles mosquito. Latent infections of some species may occur due to hypnozoites stored in the liver. P. knowlesi is morphologically indistinguishable from P. malariae on blood film preparations.
24 Hours Mon - Fri
% parasitaemia (applicable to P. falciparum & P. knowlesi infection)
No reference ranges applicable.
Genus and species reportable.
Blood parasitology - malaria
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
Serum, Serum separator.
Plasma:
Potassium EDTA, Lithium heparin, Sodium heparin, Ammonium heparin
20-25℃: 24 hrs
2-8℃: 48 hrs
-20℃: 3 months
Abbott IFU
24 hours
ug/L
Adult (fasting, 12hours): 0.80-5.20
Adult (postprandial): 2.0 - 9.0
C-peptide
Abbott Alinity c, Turbidimetric/ Immunturbidimetric
Serum:
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin (with or without gel barrier)
Sodium heparin
EDTA
20-25℃: 15 days
2-8℃: 2 months
-20℃: 1 year
Pearson TA et al, Circulation 2003; 107:499-511
24 hours
mg/L
Adult: < 5.0
Lowest relative CVD risk: < 1.0
Average relative CVD risk: 1.0 - 3.0
Highest relative CVD risk: > 3.0
C-reactive protein - high sensitivity
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
Serum, Serum separator.
Plasma:
Tripotassium EDTA, Sodium Heparin,
Lithium Heparin
2-8℃: 7 days
-20℃: longer
Abbott IFU
24 Hours
U/mL
Adult: < 35
CA 125
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
Serum, Serum separator.
Plasma:
Tripotassium EDTA, Sodium Heparin,
Lithium Heparin
2-8℃: 7 days
-20℃: longer
Abbott IFU
24 hours
U/mL
Adult: < 31.3
CA 15-3
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
Serum, Serum separator.
Plasma:
Tripotassium EDTA, Sodium Heparin,
Lithium Heparin
2-8℃: 7 days
-20℃: longer
Abbott IFU
24 hours
U/mL
Adult: <37
CA 19-9
Abbott Alinity c Spectrophotometry, Arsenazo III
Serum:
Serum separator tubes
Plasma:
Lithium heparin, Sodium heparin
Urine:
Random or 24 hour
Serum:
20-25°C: 3 days
2-8°C: 3 weeks
-20°C: 8 months
Urine:
20-25°C: 4 days
2-8°C: 7 days
-20°C: 3 months
Serum: In-house study "September 2022, PSM version 5.02" as per Dr Michael Louw, 26-08-2025
Urine: Abbott IFU
24 Hours
mmol/L
Serum:
upto 1 month: 1.9 - 2.5
upto 1 year: 2.1 - 2.7
upto 4 year: 2.1 - 2.6
upto 20 year: 2.3 - 2.75
Adult: 2.1 - 2.6
Urine:
Pediatric: Up to 0.15 mmol/kg/day
Adult Ca-free diet: 0.13 - 1.00 mmol/day
Adult Ca diet: 2.50 - 7.50 mmol/day
Random - male: 0.23 - 9.48 mmol/L
Random - female: 0.13 - 8.93 mmol/L
Calcium
CALCULATION based on Abbott Alinity methodologies for Calcium and Albumin. FORMULA:
Serum:
Serum tubes (with or without gel barriers)
Plasma: Acceptable anticoagulants:
Lithium heparin, Sodium heparin
20-25℃: 7 days
2-8℃: 3 weeks
-20℃: 8 months
Abbott IFU
24 hours
mmol/L
Adult: 2.1 - 2.55
Calcium, calculated
Abbott Alinity c Spectrophotometry, Arsenazo III
Spot Urine
or
Timed Specimen (24hours)
20-25℃: 2 days
2-8℃: 4 days
-20℃: 3 weeks
Abbott IFU
24 hours
mmol/L
mmol/24hr
Adult Male: 0.23 to 9.47
Adult Female: 0.13 to 8.92
Calcium free: 0.13 to 1.00
Low to average: 1.25 to 3.75
Average (20 mmol/day): 2.5 to 7.5
Calcium-urine
Fluoroenzyme immunoassay on Phadia 250 - Phadia EliA 2nd Generation
At least 20g stool sample.
Temperature: + 4ºC or room temp or frozen
Stool: 8 days RT or at 2°C to 8°C.
The stool extract can be stored at room temperature for a max 3 days, at +4℃ for 7 days and at <=20℃ for 3 months.
- Phadia Calprotectin 2 IFU
- “EliA Calprotectin Assay Background Technical & Clinical 15.11.2012”, presentation from ThermoFisher.
- NICE guideline DG11.
Calprotectin is a calcium- and zinc-binding protein which is predominantly present in the cytoplasm of cells involved in pathogen defence, such as neutrophil granulocytes, monocytes and macrophages. In neutrophil granulocytes it accounts for as much as 60% of the cytosolic protein. In intestinal inflammation neutrophil granulocytes migrate through the intestinal wall into the intestinal lumen, which leads to an elevated calprotectin level in the stool. The level of faecal calprotectin correlates directly with the number of neutrophil granulocytes in the intestinal lumen and is thus specifically elevated in inflammatory bowel diseases (IBD), such as Crohn's disease and ulcerative colitis, and to a much smaller extent in other entities such as neoplasia and polyps. Faecal calprotectin measurement is an easy, non-invasive first line test which clearly differentiates IBD from IBS (irritable bowel syndrome) and other functional disorders. It has been shown to be the most sensitive and most specific test for this discrimination; clearly outperforming blood tests such as CRP or ESR. Faecal calprotectin correlates with disease activity and is able to predict relapses in IBD. This makes faecal calprotectin useful for both diagnosis and monitoring of IBD patients.
2 weeks maximum (batched).
<50 ug/g: Negative. Calprotectin level not suggestive of organic pathology.
50-100 ug/g: Gray Zone. Organic pathology cannot be excluded. A repeat sample in 4 to 6 weeks is suggested.
>100 ug/g: Positive. Calprotectin level is consistent with organic pathology.
Calprotectin (faeces)
Abbott Alinity c Enzymatic Immunoassay
Urine Clean plastic or glass container
2-8℃: 5 days
-20℃: longer
Abbott IFU
24 hours
ng/mL
Positivity Cut-off: 50
Cannabinoids, semiquantitative
Abbott Alinity c Spectrophotometry, PEP Carboxylase
Serum :
Serum tubes (with or without gel barrier)
20-25°C: 2 hours
2-8°C: 2 days
Abbott IFU
24 Hours
mmol/L
Adult: 22 to 29 > 60 years 23 to 31
Carbon dioxide/ bicarbonate
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
Serum, Serum separator.
Plasma:
Sodium heparin, Lithium heparin,
Potassium EDTA
2-8℃: 7 days
-20℃: longer
Abbott IFU
24 hours
ng/mL
Adult: <5
Carcino embryonic antigen CEA
Abbott Alinity c Turbidimetric/ Immunturbidimetric
Serum: Serum tubes (not gel tubes)
Plasma: Lithium heparin (not gel tubes)
20-25℃: 8 days
2-8℃: 2 weeks
-20℃: 3 months
Abbott IFU
24 hours
g/L
Adult: 0.2 to 0.6 g/L
Ceruloplasmin
The cobas® 4800 CT/NG Test is an in vitro nucleic acid amplification test for the qualitative detection of Chlamydia trachomatis (CT) and/or Neisseria gonorrhoeae (NG) in patient specimens. The test allows for detection of CT/NG DNA in endocervical and vaginal swab specimens, and male and female urine in cobas® PCR Media. The intended targets for the cobas® 4800 CT/NG Test include all fifteen major Chlamydia trachomatis serovars, the Swedish C. trachomatis mutant (nvCT), and both wild-type and variant DR-9 sequences of N. gonorrhoeae.
Urine or urine in cobas PCR Urine Media (cobas® PCR Urine Sample Kit).
Endocervical or Vaginal swabs in cobas PCR Media (cobas® Media Dual Swab Kit).
Urine specimens should be transferred into the cobas PCR media tube as soon as possible. If specimens cannot be transferred immediately, they can be stored at 2-30℃ for up to 24 hours. Stabilised urine specimens are stable at 2-30℃ for up to 12 months.
Swabs collected with the cobas PCR Media Swab Kit may be stored at 2-30℃ for up to 12 months.
Cobas® 4800 CT/NG Test Method Sheet Doc. Rev. 19.0.
Chlamydia trachomatis (CT) is the second most leading cause of sexually transmitted diseases worldwide, with approximately 89.1 million cases occurring annually worldwide. CT is the causative infectious agent for a variety of diseases in men, including urethritis, proctitis, conjunctivitis and epididymitis. In women, the consequences of infection with CT are severe if left untreated. Infection can lead to endometriosis, salpingitis (with subsequent infertility and ectopic pregnancy) and perihepatitis. Additionally, infants from infected mothers can develop conjunctivitis, pharyngitis, and pneumonia.
Neisseria gonorrhoeae (NG) is the causative agent of gonorrhoeae. Acute urethritis is seen in the majority of men with gonorrhoeae, and acute epididymitis is the most common complication, particularly in young men. In women, the primary site of infection is the endocervix, there’s a high prevalence of coinfections with CT, Trichomonas vaginalis, and bacterial vaginosis. Many women remain asymptomatic; when symptoms do occur, the most common are increased discharge, dysuria, and intermenstrual bleeding. Additionally, NG may cause pelvic inflammatory disease, endometriosis, tubo ovarian abscess, and pelvic peritonitis.
Preparation of patient: Prior to the collection of urine, the patient should not have urinated for at least one hour. For best results, female patients should not cleanse the labial area prior to collection.
There is no physical preparation for the vaginal swab.
Precautions: None for patient. Media contains Guanidine Thiocyanate, adequate PPE for the person taking the sample.
Note: Chlamydia trachomatis and Neisseria Gonorrhoeae are notifiable diseases under the Infectious Diseases (Amendment) Regulations 2020 (S.I. No. 53/2020).
4 working days from sample receipt
CT and/or NG Detected
Not Detected
Invalid
Chlamydia Trachomatis & Neisseria Gonorrhoeae (CT/NG)
Abbott Alinity c Indirect ISE
Serum:
Serum tubes (with or without gel barrier)
For Potassium, hemolyzed specimens must not be used.
Plasma: Acceptable anticoagulants are:
Lithium heparin (with or without gel barrier)
Sodium heparin
20-25℃: 7 days
2-8℃: 7 days
-20℃: 1 year
Abbott IFU
24 Hours
mmol/L
Adult: 98 - 107
Chloride
Abbott Alinity c, Selective resolution of LDL-Particles under dye formation
Serum :
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin, Sodium heparin, EDTA Anticoagulants containing citrate should not be used.
2-8℃: 5 days
-80℃: 3 months
Source: ESC/EAS Guidelines for the management of dyslipidaemias. http://www.eassociety.org/guidelines-2.aspx
24 Hours
mmol/L
0.0 – 3.0
Cholesterol, LDL (direct)
Abbott Alinity c Enzymatic
Serum: Serum separator
Plasma Lithium heparin
Lithium heparin separator
Sodium heparin
20-25℃: 7 days
2-8℃: 7 days
-20℃: 3 months
Source: ESC/EAS Guidelines for the management of dyslipidaemias. http://www.eassociety.org/guidelines-2.aspx
24 hours
mmol/L
Adult: < 5.0
Cholesterol, total
Abbott Alinity c, Accelerated enzymatic Reaction/selective solvent
Serum :
Serum tubes (with or without gel barrier)
Plasma Collection tubes Acceptable anticoagulants are:
Lithium heparin, Sodium heparin, EDTA
20-25℃: 7 days
2-8℃: 7 days
-20℃: 1 year
National Cholesterol Education Program (NCEP) Adult Treatment Panel III Report and European Guidelines http://www.eassociety.org/guidelines-2.aspx
24 Hours
mmol/L
Adult: >1.0
Cholesterol, ultra HDL
The BD MAX Cdiff assay performed on the BD MAX System is an automated in vitro diagnostic test for the direct, qualitative detection of the Clostridioides difficile toxin B (tcdB) gene in human liquid or soft stool specimens from patients suspected of having Clostridioides difficile infection. The test, performed directly on the specimen, utilises real-time polymerase chain reaction (PCR) for the amplification of Clostridioides difficile toxin B DNA and fluorogenic target-specific hybridisation probes for the detection of the amplified DNA.
Sample Type: Liquid or soft stool
Minimum Volume: 10μL
Temperature:
- 2°C - 25°C for up to 48 hours (2 days)
- 2°C - 8°C for up to 120 hours (5 days)
2°C - 25°C for up to 48 hours (2 days)
2°C - 8°C for up to 120 hours (5 days)
Laboratory Sample Storage
Primary Sample: 7 days at 2°C - 8°C
Sample Buffer Tubes: 5 days at 2°C - 8°C
Source: BD MAX Cdiff REF 442555 P0215(07) 2023-11
Clostridioides difficile is an anaerobic, gram-positive bacillus that is the leading cause of antibiotic associated diarrhoea and pseudomembranous colitis in health care facilities. Incidence of Clostridioides difficile infection has been increasing, and severe cases are becoming more common. Disease symptoms range from mild diarrhoea to sever colitis, and even bowel perforation and death. The most common risk factor is exposure to antibiotics.
The BD MAX Cdiff assay performed on the BD MAX System is an automated in vitro diagnostic test for the direct, qualitative detection of the Clostridioides difficile toxin B (tcdB) gene in human liquid or soft stool specimens from patients suspected of having Clostridioides difficile infection. The test, performed directly on the specimen, utilises real-time polymerase chain reaction (PCR) for the amplification of Clostridioides difficile toxin B DNA and fluorogenic target-specific hybridisation probes for the detection of the amplified DNA.
PCR methods for the detection of toxin B (or toxin A) have been developed with high sensitivity and specificity as compared to cell cytotoxicity and immunoassays. Additionally, the PCR test can be performed in less than 3 hours. The combination of these characteristics may allow for prompt targeted treatment of patients with Clostridioides difficile infection and thus potentially improve patient outcome, reduce recovery time, and improve infection control practices.
3 working days from sample receipt
Toxigenic Clostridioides difficile Detected
Toxigenic Clostridioides difficile Not Detected
Invalid
Clostridioides Difficile PCR
Abbott Alinity c, Enzyme immunoassay
Urine Clean plastic or glass container
2-8℃: 5 days
-20℃: longer
Abbott IFU
24 hours
ng/mL
Positivity Cut-off: 300
Cocaine, semiquantitative
Abbott Alinity c Immunoturbidimetry
Serum: Serum tubes (with or without gel barrier)
Plasma - Acceptable anticoagulants are: Lithium heparin (with or without gel barrier) Sodium heparin
2-8℃: 3 days
-20℃: 8 days
Abbott IFU
24 hours
g/L
Adult Male 14 - 80 years: 0.82 - 1.85
Adult Female 14 - 80 years: 0.83 - 1.93
Complement C3
Abbott Alinity c Immunoturbidimetry
Serum:
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin (with or without gel barrier)
Sodium heparin
EDTA
2-8℃: 2 days
-20℃: 2 days
Abbott IFU
24 hours
g/L
Adult Male 14 - 80 years: 0.15 - 0.53
Adult Female 14 - 80 years: 0.15 - 0.57
Complement C4
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum:
Serum, Serum separator.
Plasma: Lithium Heparin, Sodium Heparin,
Potassium EDTA
Plasma separator tubes with Lithium Heparin.
2-8℃: 14 days
-20℃: 30 days
Blood: Handbook of Diagnostic Endocrinology, 2nd Edition, 2008. William E Winter & al. AACC Press
24 hours
nmol/L
Morning 08:00H: 171 - 800
Afternoon: Approx. half the morning values
In the evaluation of Adrenal
Highly Unlikely: >550
Virtually Diagnostic <138
Evening 24H00:
Virtually excludes: <138
Highly suggestive: <207
Cortisol
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Urine: The urine sample must be collected in a clean, previously unused container.
Preservatives are not required; however, ten grams of boric acid per liter of urine may be used.
2-8℃: 14 days
-20℃: 30 days
Abbott IFU
24 hours
nmol/24hr
Adult: 12 - 486
Cortisol - urinary
Abbott Alinity c, NAC (N-Acetyl-L-Cystein)
Serum:
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants:
Lithium heparin
20-25℃: 2 days
2-8℃: 7 days
Abbott IFU
24 Hours
U/L
Adult Male: 30 - 200
Adult Female: 29 - 168
Creatine kinase CK
Abbott Alinity c, Enzymatic
Serum:
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin
20-25℃: 7 days
2-8℃: 7 days
-20℃: 3 months
Abbott IFU
24 hours
µmol/L
Adult Male: 64 - 104
Adult Female: 49 - 90
Creatinine enzymatic
Fluoroenzyme immunoassay on Phadia 250. SOP: CC99
Tube Type:
Serum (Red and gold cap);
Heparin (Green cap) or EDTA
(Lavender cap) Plasma
Stability Whole blood: RT unknown. 7 days @ + 4°C
Phadia IFU
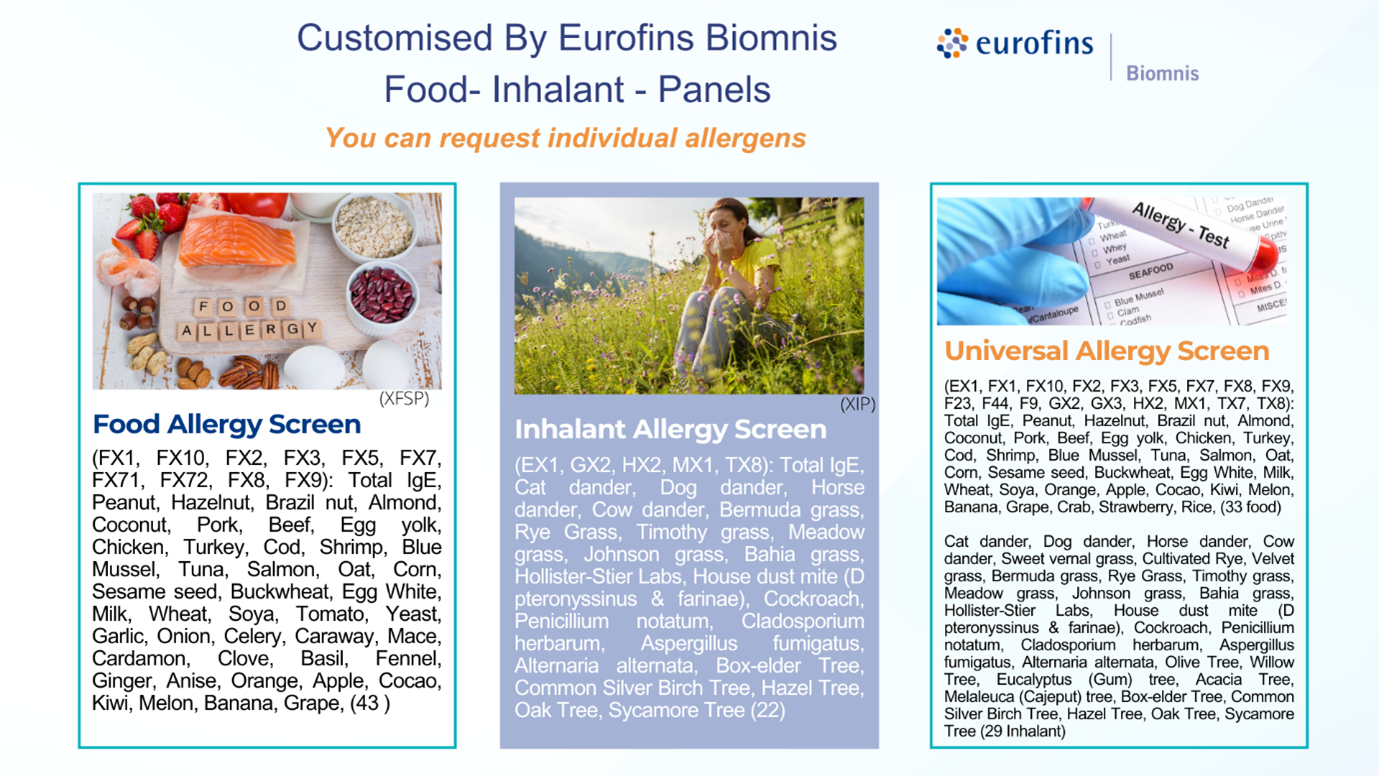
Having taken a thorough medical history and clinical symptoms, you may have a strong suspicion and decide against the Alex Allergy in favour of our customised allergy panels; Food Allergy Screen, Inhalant Allergy Screen or the Universal Allergy Screen.
Preparation of Patient: There is no special physical preparation for specific IgE analysis.
Location: Eurofins Biomnis Blackthorn Road
4 working days
Panels are reported as Positive or Negative only.
Individual allergens are reported in kIU/L, ranging from less than 0.10 to greater than 100. A result of > 0.10 kIU/L is interpreted as positive.
Customised Allergy Panels
Cytology Processing. Diagnosis.
- An adequately completed test request form must accompany the specimen.
- Fluid should be freshly collected and placed into:
- a container with an equal volume of CytoRich Red Collection Fluid, or The specimen container(s) must be adequately labelled.
- an empty sterile container and kept refrigerated
- Up to 20mls of the fluid is an adequate volume for testing.
- The aspirated material should be spread onto a glass slides and air dried or fixed (fixative available from the lab)
- If a needle rinse is available, it should be collected into a container with CytoRich Red Collection Fluid.
- All slides must be labelled with patient name and date of birth written using pencil on the frosted end of the slide.
If transport of the specimen will be delayed for more than 24 hours, the cytofix should be added at collection. The specimen is stable for 48 hours if stored at 4 degrees .
A range of fluid types can be collected from the body including urine, cyst fluid, pleural fluid, and ascetic fluid.
Cytology specimens can be sent to the laboratory in conjunction with a histopathology specimen or in isolation. Collecting a cytology specimen can be less invasive than sampling for a histopathology specimen, but there are associated limits in the diagnostic value of a cytology specimen.
Fine needle aspiration of mass lesions is commonly utilized in the detection and characterization of a variety of malignant diseases. Obtaining an adequate specimen requires attention to good aspiration technique as well as processing of material obtained. It is highly desirable that several direct smears are prepared (preferably air-dried) for all fine needle aspiration specimens submitted to the laboratory.
10 working days
Cytology specimens
Chemiluminescent microparticle immunoassay (CMIA)
Chemiluminescent microparticle immunoassay (CMIA)
Serum (Gold and red cap);
Plasma (green and lavender cap)
Temperature: + 4ºC
Miscellaneous: Non fasting
Serum (Gold and red cap);
Plasma (green and lavender cap)
Temperature: + 4ºC
Miscellaneous: Non fasting
Whole blood: RT unknown; ≤14 days 2-8ºC
Separated: RT unknown; ≥14 days -10°C or colder
Whole blood: RT unknown; ≤14 days 2-8ºC
Separated: RT unknown; ≥14 days -10°C or colder
Source: Abbott IFU
Source: Abbott IFU
Infections with CMV (a member of the herpes virus family) are very common and usually mild and asymptomatic. In immunocompromised patients, however, infections can be severe and sometimes fatal. Also, in utero infection of the
foetus can lead to birth defects. If the CMV IgG is positive, CMV IgM is measured to determine if the infection is current or recent.
Preparation of Patient: There is no special physical preparation for these tests.
3 working days
3 working days
CMV IgG:
≥6.0 AU/mL are considered reactive (POSITIVE)
Less than 6.0 AU/mL are nonreactive (NEGATIVE)
CMV IgM:
Index <0.85 are considered nonreactive (NEGATIVE)
Index 0.85 to 0.99: GRAYZONE, Repeat in 7 to 14 days
Index greater than or equal to 1.00: reactive (POSITIVE)
Cytomegalovirus IGG and IGM antibodies
Stago Compact Max
Sodium Citrate 3.2%,
Temperature: 8 hours Room temperature or 2 weeks at -20ºC
Miscellaneous: N/A
Whole blood: 8 hours, unless centrifuged at room temperature at 1500 RCF for 15 min, separated and the plasma frozen. Can only be thawed once. If an expected delay from collection time to receipt in the laboratory, suggest send frozen plasma.
Ref: (BD Ref. VS5966 Evaluation of 0.109M BD Vacutainer® Plus Plastic and 0.105M BD Vacutainer® Glass Sodium Citrate Tubes for PT and APTT Using the Sysmex CA - 1500 Analyzer. BD, Franklin Lakes, NJ, USA June 2002; CLSI H21-A5)
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings CS, Jiménez D, Kucher N, Lang IM, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Áinle FN, Prandoni P, Pruszczyk P, Righini M, Torbicki A, Van Belle E, Zamorano JL; The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J. 2019 Oct 9;54(3):1901647. doi: 10.1183/13993003.01647-2019. PMID: 31473594.
D-dimer is a degradation product of cross-linked fibrin. The D-dimer concentration is a measure of the fibrinolytic activity of plasmin in the vascular system. Elevated concentrations of D-dimer indicate increased coagulatory and fibrinolytic activity. With a normal D-dimer value, acute deep vein thrombosis and pulmonary embolisms may be ruled out with high reliability.
Preparation of patients: There is no physical preparation for the D-Dimer test.
Precautions: No modifications to change diet, medications, or activity required before this test. Phlebotomists should enquire about any blood thinners or anticoagulant medication any diseases like liver disease and rheumatoid arthritis. There are some herbs that are also able to replicate the effects of blood thinning medication.
SAME DAY
µg/mL
0.0-0.50
D-Dimer
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator.
Plasma: Potassium EDTA,
Sodium citrate
Sodium heparin
2-8℃: 8 days
-20℃: longer
Abbott IFU
24 hours
µmol/L
Male: 19Y 1.2 -10.4
Male: 24Y 6.5 -14.6
Male: 34Y 4.6 -16.1
Male: 44Y 3.8 -13.1
Male: 54Y 3.7 -12.1
Male: 64Y 1.3 -9.8
Male: >64 6.2 -7.7
Female: 19Y 1.7 -13.4
Female: 24Y 3.6 -11.1
Female: 34Y 2.6 -13.9
Female: 44Y 2 -11.1
Female: 54Y 1.5 -7.7
Female: 64Y 0.8 -4.9
Female: >64 0.9 -2.1
Dhea-S
Abbott Alinity c, Particle-enhanced turbidimetric inhibition immunoassay (PETINIA)
Serum :
Serum tubes (with or without gel barrier)
Plasma: Acceptable anticoagulants are:
Lithium heparin
Sodium heparin
Potassium EDTA
Heparin gel plasma separator
2-8℃: 48 hours
-20℃: 7 days
Therapeutic range for digoxin as recommended by European Society of Cardiology Guidelines for the diagnosis and treatment of acute and chronic heart failure.
European Heart Journal (2008) 29, 2388 - 2442.)
24 hours
ug/L
0.6 – 1.2
>2 associated with toxicity
Digoxin
TACseq Illumina Inc. technology based on sequencing by NGS.
Endometrial tissue/liquid
Drop Biopsy RNALater Cryotube.
Cool +4 O/N and Ship at RT within Max 4 days
e-Ready is a predictive molecular test that assesses endometrial receptivity by analysing the expression of 68 genes from an endometrial biopsy. It identifies the personalised window of implantation to optimize embryo transfer timing in ART cycles, particularly in cases of recurrent implantation failure.
18 days
E-ready
Abbott Alinity c Immunalysis assay
Urine Clean plastic or glass container
20-25℃: 7 days
2-8℃: 2months
-20℃: >2months
Immunalysis EDDP IFU
24 Hours
g/ml
Positivity Cut-off: 100
EDDP methadone metabolite
CALCULATION based on Creatinine methodology and patient demographics.
Serum Serum tubes (with or without gel barrier)
Plasma -Acceptable anticoagulants are: Lithium heparin (with or without gel barrier) Sodium heparin EDTA is not recommended.
20-25℃: 7 days
2-8℃: 7 days
-20℃: 3 months
https://kdigo.org/
24 hours
Adults:
> 90: Normal
60 - 89: Normal or Stage 2 CKD
30 - 59: Moderate
EGFR
Abbott Alinity c, Enzyme immunoassay
Urine Clean plastic or glass container
2-8℃: 5 days
-20℃: longer
Abbott IFU
24 Hours
ng/mL
Positivity Cut-off: 500
Ecstasy, semiquantitative
Next Generation Sequencing
Embryosafe assess embryo health by testing for aneuploidies (PGT-A), chromosomal structural abnormalities (PGT-SR), and monogenic diseases (PGM-M). It helps identify the most viable embryos, reducing the risk of miscarriage and genetic disorders.
PGT-A detects chromosomal abnormalities such as trisomy and monosomy, improving implantation success and reducing miscarriage rates in IVF. It also identifies mosaic embryos, which contain both euploid and aneuploid cells, guiding embryo selection.
PGT-SR identifies chromosomal structural rearrangements that can cause infertility, miscarriage or congenital abnormalities.
PGT-M screens for monogenic diseases such as cystic fibrosis, for selecting embryos free from inherited genetic disorders.
niEmbryoSafe
niEmbryoSafe is a non-invasive test that analyses cell-free embryonic DNA from spent culture media to assess chromosomal status without embryo biopsy, offering a viable alternative to traditional PGT-A.
PGT-A Next (the Ploidy test)
PGT-A Next for Ploidy extends traditional PGT-A/SR by analysing chromosomal ploidy, identifying embryos with a normal diploid set, even if they initially appeared morphologically abnormal. It is indicated for abnormal fertilisation patterns, previous polyploid or triploid pregnancies, recurrent miscarriages linked to polyploidy or suspected diploid anomalies in IVF embryos.
24h for fresh transfer / 9-11 days for frozen embryos
Embryosafe
DNA extraction and NGS analysis
Endometrial biopsy or fluid collected between the 15th and 25th day of the natural cycle or during the secretory phase in case of hormone replacement therapy.
Endometriome assesses the endometrial microbiome to identify imbalances that may affect implantation, measuring lactobacilli levels and detecting chronic endometritis. Early detection of altered endometrial microbiota enables personalised treatments to improve implantation rates in infertile patients.
18 days
Endometriome
Haematology – Capillary photometric-kinetic technology
Whole Blood K2/K3 EDTA anticoagulated.
2 days @ + 2-8ºC
Reference ranges for the ESR assay are derived in house. Data was obtained from a clinical normal population and statistics generated using the Graph Pad statistics module. Data was analysed for Gaussian distribution and reference ranges derived using either parametric or non-parametric statistics. A copy of the data is kept in the QA department.
The Erythrocyte Sedimentation Rate (ESR) is a blood test which measures the rate at which red blood cells (erythrocytes) settle at the bottom of a tube over a specific period, usually 1 hour. The ESR is affected by the presence of plasma proteins, such as fibrinogen, IgM, alpha2-macroglobulin and other acute phase proteins, which encourage erythrocyte agglomeration. It is important to note that while ESR is a useful tool, it is not specific to any particular disease. A high ESR can be seen in various conditions, and additional tests are often needed to achieve an accurate diagnosis. The ESR, therefore, forms a part of a broader spectrum of diagnostic tools which healthcare professions use to assess and monitor inflammatory and infectious disease.
Preparation of patients: There is no physical preparation for the ESR test.
Precautions: The ESR should not be used to screen healthy persons for disease.
24 Hours
mm/hr
Male:
>50 Years: 0 - 12
<50 Years: 0- 8
Female:
>50 Years: 0 - 15
<50 Years: 0 - 10
Erythrocyte sedimentation rate
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator Plasma: Lithium heparin, Plasma separator, Potassium EDTA
2-8℃: 7 days
-20℃: longer
Abbott IFU
Estradiol regulates the menstrual cycle, follicular development, ovulation and endometrial preparation for implantation. It is used to assess ovarian reserve, monitor ART cycles, and guide fertility management. In males, estradiol imbalances can impair spermatogenesis and contribute to infertility.
24 Hours
pmol/L
Follicular phase: 77 – 922
Mid Cycle phase: 140 – 2383
Luteal phase: 77 – 1145
Postmeno pausal no HRT: < 103
Postmeno pausal on HRT: < 529
Male: 40 – 161
Estradiol
Abbott Alinity c Enzymatic (Alcohol Dehydrogenase)
Urine Clean plastic or glass container
2-8℃: 30 days
-20℃: longer
Abbott IFU
24 Hours
mg/dL
Positivity Cut-off: 10
Ethanol
Gene expression profiling.
Vaginal & Endocervical swabs
Eubiome analyses the vaginal microbiome by quantifying key lactobacillary species and detecting opportunistic pathogens, STI’s and high-risk HPV. It classifies the microbial profile into one of five Community State Types, providing a dynamic assessment of eubiosis or dysbiosis. Eubiome aids fertility assessment by identifying microbiota imbalances that may affect implantation or contribute to recurrent miscarriage, guiding personalised clinical strategies based on microbial composition.
10 - 13 days
Eubiome
OC-Sensor Pledia, Latex Agglutination Immunoturbidimetry
Faeces sample collected into an analyser specific sampling bottle containing buffer (OC Auto Sampling Bottle 3).
2-8℃: 10 days
BowelScreen Guidelines for Quality Assurance in Colorectal Screening, Second Edition, Published 2017, ISBN 978-1-907487-26-2
24 Hours
ng/ml
Normal range cutoff: <100
NSS Bowel Screen Normal Range Cutoff: <225
Faecal immunochemical test (FIT)
1 mL Serum or Heparin Plasma
Luteinising Hormone (LH)
Follicle Stimulating Hormone (FSH)
Prolactin
Oestradiol
Progesterone
Female Infertility Profile
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator
Plasma: Tri potassium EDTA, Lithium heparin
2-8℃: 7 days
-20℃: 1 year
Abbott IFU
24 Hours
ng/mL
Adult Male: 15- 200
Adult Female: 15 - 150
4 - 14 days (M/F): 12 – 717
15 days - <6 months (M/F): 12 - 647
6 months to <1 year (M/F): 12 – 182
1 to <5 years (M/F): 12 - 100
5 to <14 years (M/F): 15 - 79
14 to <19 years (F): 15 - 67
14 to <16 years (M): 15 - 83
16 to <19 years (M): 15 - 172
Ferritin
Next Generation Sequencing
3ml Blood
Fertiscan offers an innovative genetic analysis of infertility in both males and females. Using NGS, it investigates over 70 genes associated with primary ovarian insufficiency, ovarian dysfunction, ovarian dysgenesis, recurrent miscarriage, oocyte maturation defects, and other reproductive disorders. In males, more than 50 genes linked to spermatogenesis defects, including azoospermia, asthenospermia and abnormal sperm morphology, are analysed.
Fertiscan is indicated for couples with unexplained infertility, recurrent miscarriage, or repeated ART cycle failure.
17-22 days
Fertiscan
Stago Compact Max, Stago Satellite Max
Sodium Citrate Plasma 3.2% 0.105M
Temperature: 4 hours Room temperature or 2 weeks @ -20ºC.
If an expected delay in transporting samples to the laboratory samples should be centrifuge, separated & send as frozen within 4 hours of blood collection.
Miscellaneous: N/A
Collection: Cf. Special requirement for Coagulation test
Whole blood: 4 hours, unless centrifuged at room temperature at 1500 RCF, separated and the plasma frozen. Can only be thawed once. If an expected delay from collection time to receipt in the laboratory, suggest send frozen sample.
Ref: CLSI H21-A5)
Dacie and Lewis, Practical Haematology 12th edition, 2017
Clauss developed a simple method for the quantitative determination of Fibrinogen by measuring the clotting time of dilute plasma after the addition of Thrombin. The clotting time is inversely proportional to the Fibrinogen concentration. The clotting time obtained in this manner is then compared with that of a standardised Fibrinogen preparation. The plasma must be diluted to provide a low level of potential inhibitors, e.g. FDP’s and Heparin. A strong Thrombin solution is utilised in order to ensure that the clotting time is independent of Thrombin concentration over a broad range.
Preparation of patients: Patients should be relaxed pre-venepuncture. Excessive stress and exercise will increase Factor VIII, vWF antigen and fibrinolysis. Veno-occlusion should be avoided.
Precautions: This test is not recommended for patients with active bleeding, acute infection or illness, or in those patients who have received blood transfusions within four weeks. Drugs that may increase Fibrinogen levels includec estrogens and oral contraceptives. Drugs that may cause decreased levels include anabolic steroids, androgens, Phenobarbital, Urokinase, Streptokinase, and Valproic acid.
24 Hours
g/L
1.8 – 3.6
Fibrinogen (Clauss method)
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Folate:
Serum: Serum, Serum separator
Plasma: Lithium heparin plasma, Lithium heparin plasma separator.
2-8℃: 7 days
-20℃: 30 days
Abbott IFU
24 hours
ng/mL
Adults: 3.1 - 20.5 ng/mL
Folate
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator
Plasma: Sodium heparin, Lithium heparin, Potassium EDTA
2-8℃: 7 days
-20℃: 1 year
Abbott IFU
FSH, secreted by the anterior pituitary, regulates gametogenesis. In females, it promotes granulosa cell proliferation, follicular maturation, oestrogen synthesis, and the expression of LH receptors, all essential for ovulation. In males, FSH supports spermatogenesis through Sertoli cell stimulation and inhibin production. 1
24 Hours
UI/L
Follicular phase: 3.0 - 8.1
Mid Cycle phase: 2.6 - 16.7
Luteal phase: 1.4 - 5.5
Post-Meno pausal: 26.7 - 133
Males: 1.0 - 12.0
Follicle stimulating hormone FSH
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator
Plasma: Sodium heparin, Lithium heparin, Potassium EDTA
2-8℃: 6 days
-20℃: longer
Abbott IFU
24 Hours
pmol/L
Adult: 2.42 - 6.01
Free T3
Abbott Alinity i Chemiluminescent Microparticle Immunoassay (CMIA)
Serum: Serum, Serum separator
Plasma: Sodium heparin, Lithium heparin, Lithium heparin plasma separator, Potassium EDTA
2-8℃: 6 days
-20℃: longer
Abbott IFU
24 Hours
pmol/L
Adult: 9.01 - 19.05
Free T4
CALCULATION based on Abbott Alinity methodology for Testosterone and SHBG
Serum: Serum, Serum separator
Plasma: Lithium heparin,
2-8℃: 8 days
-20℃: 3 months
Abbott IFU
24 Hours
Male: 20.4 - 81.2
Female (Pre-meno pausal): 0.5 - 7.3
Female (Post-meno pausal): 0.6 - 8.0
Free androgen index FAI
Sysmex XN2000
Sysmex XN1000
Whole Blood K2/K3 EDTA anticoagulated.
Temperature: + 2-8ºC
Miscellaneous: N/A
Whole Blood EDTA
Temperature: + 4ºC
Miscellaneous: N/A
2 Days @ + 2-8ºC
2 Days @ + 2-8ºC
Dacie and Lewis, Practical Haematology 12th edition, 2017
Dacie and Lewis, Practical Haematology 12th edition, 2017
The Full Blood Count (FBC) is one of the most commonly requested laboratory tests, which focusses on the assessment of the cellular composition of peripheral whole blood. FBC results encompass the enumeration and specific characteristics of erythrocytes, leukocytes and platelets. Test results may provide insights into various clinical conditions, including anaemia, inflammatory response, specific neoplasms and bone marrow related disorders. The interpretation of FBC parameters should be considered in relation to the patient’s overall health, medical history, and specific presentation.
Preparation of patients: There is no physical preparation for the FBC test.
24 hours
24 Hours
Full blood count
Abbott Alinity c, L-Gammaglutamyl-3-carboxy-4-nitroanilid-Substrate
Serum: Serum separator
Plasma: Lithium heparin, Sodium heparin
20-25℃: 7 days
2-8℃: 7 days
-20℃: 3 months
Abbott IFu
24 Hours
U/L
Male: < 55
Female: < 38